What Is Diabetic Retinopathy?
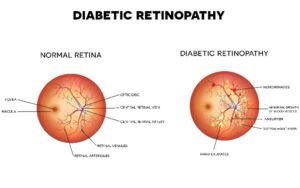
If you have diabetes, you are at risk of diabetic retinopathy, a condition that damages your retina. Over time diabetes causes the tiny blood vessels of the retina to swell, close off or leak. In some people this damage can cause irreversible vision loss.
In the earlier stages of diabetic retinopathy, known as non-proliferative diabetic retinopathy (NPDR), retinal blood vessels leak, which can lead to retinal swelling. Blood vessels can also close off, preventing blood and oxygen from reaching the retina and macula. Tiny cholesterol deposits can form, too. In the later stage of diabetic retinopathy, proliferative diabetic retinopathy (PDR), the retina tries to compensate for the lack of circulation by growing new blood vessels. These vessels are fragile and can leak blood.
If you have diabetes, it is essential that you keep up with your ocular health through routine eye examinations. Knowing the symptoms of diabetic retinopathy is also important. Should you experience any warning signs of diabetic retinopathy, you can pursue an official diagnosis and treatment intervention promptly for the best chances at saving your vision.
Diabetic Retinopathy Symptoms
Non-proliferative diabetic retinopathy may cause blurry vision that makes it difficult to read small print or focus on distant objects. For some people, this stage of the disease is asymptomatic.
Symptoms of proliferative diabetic retinopathy include reduced or blurry vision. If the new, abnormal blood vessels leak, it can create the appearance of dark floating spots called “floaters” in your vision.
Diabetic Retinopathy Risk Factors
Type 1, type 2 and gestational diabetes are the primary risk factors for diabetic retinopathy. People who have a long history of diabetes or poorly controlled diabetes are at especially high risk of getting diabetic retinopathy.
Prevention
If you have diabetes, you can reduce your risk of diabetic retinopathy by doing the following:

- Keeping your diabetes under control with the help of your medical team
- Taking diabetes medications as prescribed
- Managing blood sugar levels
- Eating a nutritional diet
- Getting plenty of physical activity
- Keeping your blood pressure and cholesterol levels in the normal range
Diagnosis
Our doctors diagnose diabetic retinopathy with an eye exam. After dilating your pupils, we will evaluate your retina for abnormal blood vessels and signs of leakage or swelling. If we officially diagnose you with diabetic retinopathy, we will keep a close eye on you and will recommend a treatment plan designed to protect you from losing vision.
Diabetic Retinopathy Treatment Options
Dr. Guri Bronner and the rest of our medical team will suggest the treatment approach that is appropriate for your circumstances. With cases of early-stage diabetic retinopathy, sometimes we recommend a “watchful waiting” approach, wherein we routinely monitor your eyes through dilated eye exams.
The more advanced stages of diabetic retinopathy can put you at higher risk for vision loss. We have the latest treatment options available at Berks Eye. With modern treatment, as long as we catch the problems early on we can prevent further loss of vision and often we can recover vision. However, the longer the disease progresses without treatment, the less likely we are to be successful. The key today is early intervention and close monitoring.
Injections of “anti-VEGF” drugs are very helpful at slowing down the progression of diabetic retinopathy. These drugs block vascular endothelial growth factor (VEGF) to inhibit the development of new, abnormal blood vessels. Laser therapy can seal off and shrink blood vessels that leak. If the bleeding is very severe, we may perform vitrectomy surgery to remove the vitreous gel, blood and scar tissue. Advances in medicine have provided us with outstanding options.
Videos
Contact Berks Eye Physicians & Surgeons Today
Our team of knowledgeable doctors offers expert diagnosis and treatment options for diabetic retinopathy. To learn more, please contact us today.
 1802 Paper Mill Road, Wyomissing, PA 19610
1802 Paper Mill Road, Wyomissing, PA 19610

